Quick Read
- Candida auris has infected over 7,000 people in 28 US states as of late 2025.
- The fungus is highly drug-resistant and spreads easily in hospitals and care facilities.
- Symptoms are often vague, making early detection and containment difficult.
In 2025, the United States is facing a formidable new threat in its hospitals and long-term care facilities: the rapid spread of a drug-resistant fungus known as Candida auris. Health officials and epidemiologists are sounding the alarm as this superbug, which has now been confirmed in at least 28 states—including Alabama, Nevada, and California—proves itself not just resilient, but elusive and deadly. The numbers tell a grim story: over 7,000 cases reported this year, quickly closing in on last year’s record-breaking 7,500, according to CDC data (Times of India, AL.com).
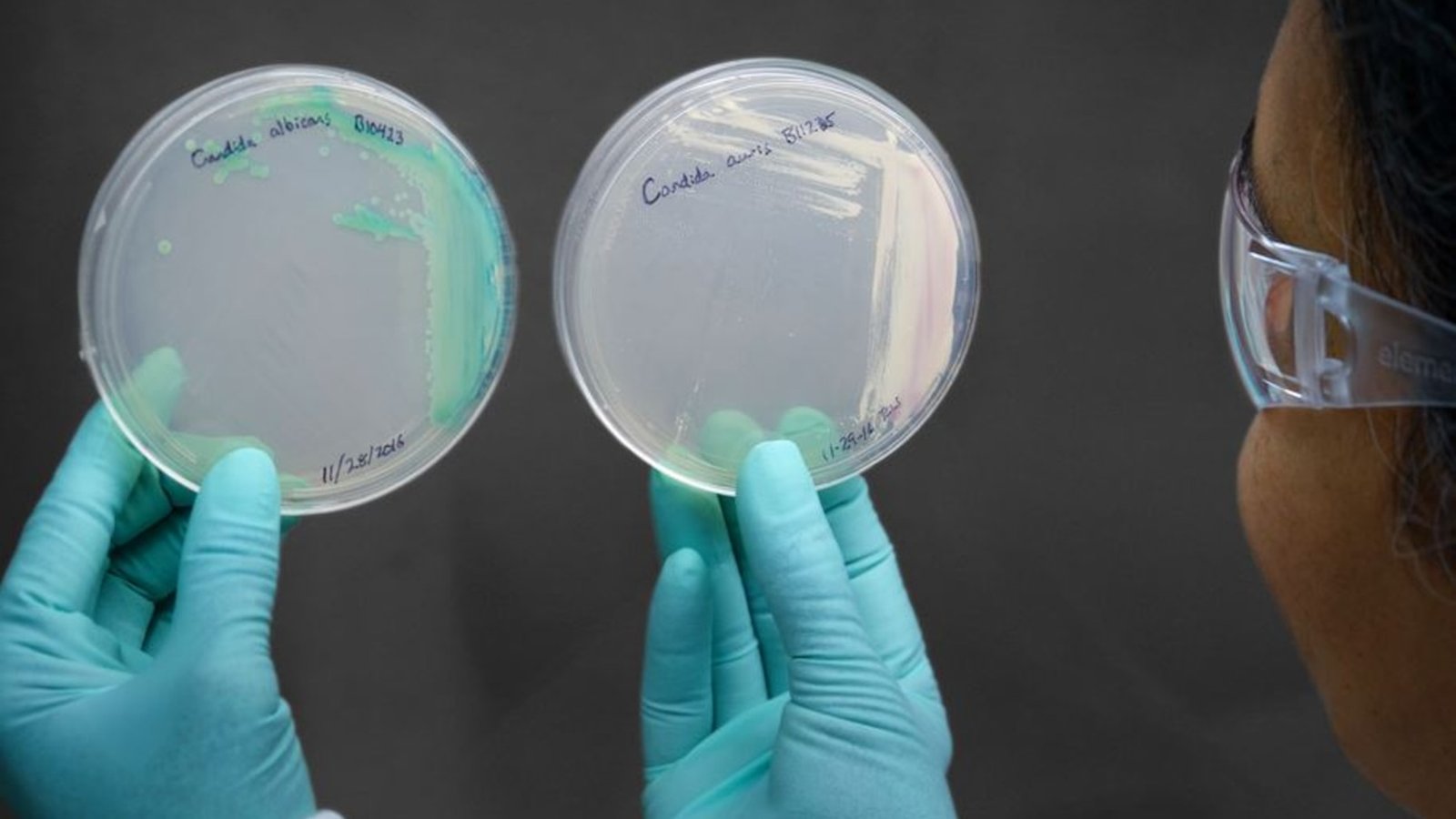
So, what exactly is Candida auris? First identified in 2009, this yeast has emerged as a global public health challenge, infecting patients in over 61 countries on six continents (Independent). Unlike more familiar fungal infections, C. auris is often resistant to multiple antifungal medications. That makes it particularly dangerous for those whose immune systems are already compromised—hospitalized patients, older adults, and long-term care residents.
The threat goes beyond drug resistance. Candida auris is a master of survival. It can live on surfaces—bed rails, medical equipment, even clothing—for months, withstanding common disinfectants and cleaning regimens. Hospitals and nursing homes, already under strain from staffing shortages and overcrowding, are finding it especially challenging to contain outbreaks. The fungus spreads easily through contaminated surfaces, shared medical equipment, and direct patient contact. Its ability to stick to skin “like glue” and form protective layers on surfaces further complicates eradication efforts (Independent).
For the average healthy person, the risk of infection remains low. But for vulnerable groups—the elderly, those in ICUs, people on ventilators or catheters, and residents of long-term care facilities—the stakes are much higher. Infection can lead to severe bloodstream, heart, or brain complications, and the mortality rate can be significant when treatment options are limited.
Symptoms of Candida auris can be frustratingly vague: fever and chills that don’t improve with antibiotics, fatigue, low blood pressure, rapid heart rate, and, in some cases, organ dysfunction. Sometimes, there may be no symptoms at all. This ambiguity means the fungus is often misidentified, delaying life-saving treatment and allowing the pathogen to spread unnoticed. In certain cases, patients may require blood transfusions, and symptoms can also include ear pain or a feeling of fullness (Times of India, AL.com).
Why is the number of cases rising now? Experts point to a perfect storm: the widespread overuse of antibiotics and antifungals, which encourages drug resistance; aging and immunocompromised populations; and healthcare systems stretched thin. Improved detection methods have also led to more cases being identified, though many likely remain undiagnosed. The Alabama Department of Public Health, for instance, highlights the challenge of unrecognized transmission within and between facilities, urging for “sustained vigilance” (AL.com).
The fungus’s biology only adds to the challenge. Candida auris possesses “efflux pumps” on its cell membrane, allowing it to eject antifungal drugs before they can act. Its ability to switch growth forms and bind tightly to human skin makes it an efficient colonizer. Colonized patients can then transmit the fungus to others, both within and between hospitals, further fueling outbreaks (Independent).
With cases confirmed in 28 states—including Oregon, California, Texas, Illinois, Pennsylvania, Georgia, North Carolina, and Alabama—the CDC and state health departments are urging aggressive containment. Measures include enhanced cleaning protocols using fungicidal disinfectants, strict hand hygiene, patient isolation, and rigorous screening of high-risk individuals. Facilities are encouraged to report cases promptly to track and limit outbreaks. But as the fungus can survive cleaning and persist on skin for months, these efforts are an uphill battle.
For families with loved ones in hospitals or nursing homes, awareness is key. Experts recommend asking about infection control practices, ensuring proper hygiene standards, and advocating for early testing if symptoms appear. While the general public faces little risk in everyday life, vigilance in healthcare settings remains essential.
The story of Candida auris is more than just a medical headline—it’s a warning about the evolving landscape of infectious diseases. As treatments lose effectiveness against superbugs, prevention and early detection become the cornerstones of public health. The fight against Candida auris is ongoing, and the response of hospitals, agencies, and policymakers in 2025 will shape the future of infection control for years to come.
The emergence and spread of Candida auris underscore a growing crisis in global health: antimicrobial resistance. As this fungus continues to evade drugs and containment, it challenges the very foundation of modern medicine. Only through coordinated, transparent action—and a commitment to vigilance—can we hope to slow its advance and protect the most vulnerable among us.